Our Services
Swift Verruca Laser Treatment
SWIFT is a new technology, developed in the UK, which has been licensed for the general treatment of skin lesions, warts & verruca in Podiatry and Dermatology. Swift uses microwave energy which is delivered through a special probe applied to the skin to treat the affected tissue.
Orthotics &/Insoles
Custom orthotics are medical prescribed devices or inserts that are placed in your footwear to support your feet, realign your hips and legs and make everyday activities like standing, walking and running more comfortable when an abnormality in your physical foot and ankle biomechanics is noted. They are sometimes referred to as orthoses, arch supports, insoles and shoe inserts.

/Podiatry & Chiropody
The podiatrists at MyFeet Clinics - the Priory Foot Clinic & the Merrion Foot clinic - will be happy to help you with any of your podiatry needs.
We treat a wide range of conditions such as Verrucas, corns, ingrown toenails, Fungal nails and much more.
Plantar Fasciitis
Heel Plantar Fasciitis is a common foot condition that predominantly affects females, older adults and athletes. It is commonly known as Plantar Heel pain or simply Heel Spurs. The pain is under the heel of your foot and is often worse first thing in the morning or as soon as you stand up after resting.
WHAT'S NEXT?
Simply book an appointment using our online booking system and we'll take care of the rest.
-
Christmas Gift Items
Gifts for a loved oneGifts for a loved one
-
Podiatric Footwear
Ladies & Mens Footwear -
Creams
To Treat your FeetA selection of creams to treat your feet.
-
Fungal Nail Treatments
Repair Fungal NailsTreat and banish Fungal Nails
-
Orthotics & Insoles
To Comfort your FeetImprove your the comfort of your shoes.
-
General Foot Care
For Healthy FeetA range of products to help improve the health of your Feet.
-
Verruca Treatments
To remove Verrucas & WartsGet rid of any Verrucas or Warts.
-
Diabetic Foot Care
Improve your Diabetic Feet.A range of products to improve Diabetic Feet.
-
One Time Payment
Make Payment Here -
Bunion Treatment
Button -
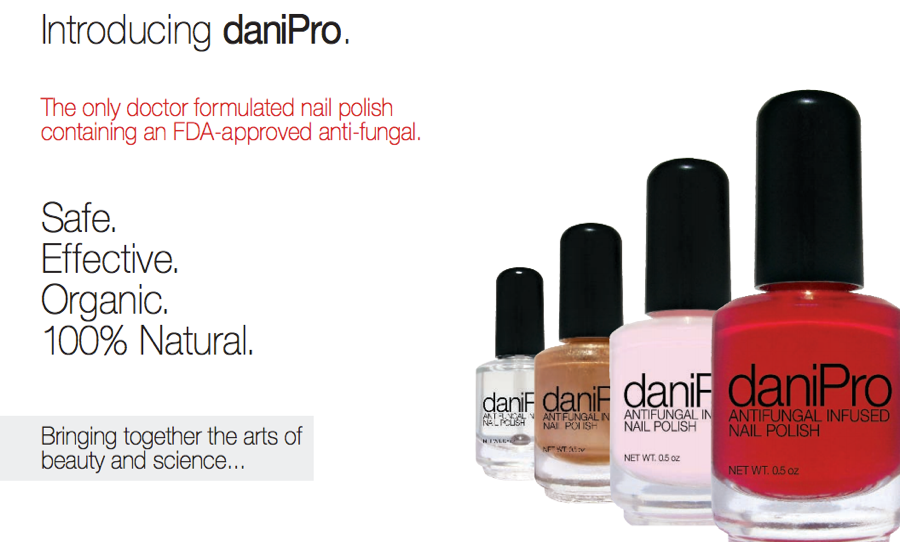
Podiatry Nail Varnish
ButtonPodiatry Nail Varnish
Our patients feedback
Consistently excellent experience and service delivery. Admin staff also are most efficient at posting appt details, receipts etc most quickly. Staff always friendly, efficient and effective. Because of circumstances I often need to change follow up appointments.
David Flynn
I have attended Merrion Foot Clinic for about five years now as a result of hereditary bad feet! After my last podiatrist retired it took me about 2 years to finally find this excellent clinic. I highly recommend this Foot Clinic.
Clodagh Bourke
Today was my second visit to the Merrion Foot Clinic,to get another bad nail removed. Joe and all the staff are really nice and go through the whole process with you beforehand. I can't recommend this clinic and Joe Eagan enough.
Denise Greene
I'm delighted with this chiropody / podiatry clinic. Joe Egan takes a holistic approach to treating feet. He took a lot of effort to ensure that my orthotics solved my specific foot problem. All the staff are efficient, friendly and reliable.
Mary Burke
Visit our Instagram for all our latest information in the clinic
-
Great day with Dr Ian Reilly on local anaesthetic. Thank you to all involved @thefarnhamfootclinic #podiatry #dublin #Ireland #podiatricmedicine #podiatricsportsmedicineButton
-
Happy St. Patricks day from MyFeet! Hope you all have a woderful day 🍀 #southDublin #medical #kneepain #diabetic #heelpainrelief #feetproblems #podiatrylife #verrucas #Podiatrist #verruca #diabeticfootcare #health #KeepingYouActiveAndPainFree #Dublin #healthyfeet #sorefeet #bunions #heel #bunion #FootCareExpert #footage #podiatrist #feet #podiatryclinic #feetcare #shoes #footcare #footproblems #runners #stpatricksdayButton
-
Podiatry Ireland CPD day Speakers James Cowden and Tommy ChanButton
-
Welcome to our team Mark Dooley Mark will be seeing patients in Athlone Foot Clinic. Mark graduated from the University of Brighton, U.K in 2014 with a BSc (Hons) degree in Podiatry. He is MChSI registered. Since 2014, he has worked in private podiatry clinics in Ireland and Australia. With a prior degree in ‘Sport Science & Health’, being qualified as a physical therapist, and having competed for many years in national-level distance running, Mark especially enjoys treating sports injuries and musculoskeletal podiatry cases.Button
-
We will be closed for Christmas 🎄 23 December until Wednesday 03 January We will open again on Thursday 04 January ✨️Button
-
GIVEAWAY worth €110 ✨️ 1st prize: €80 voucher for podiatry appointment in our clinic + €30 worth of footcare products* 2nd prize: €30 worth of footcare products * All you have to do is: ❤️Like post 💬Tag 3 friends ➡️Share our post Winners will be announced on Wednesday 20th Dec @4pm *T&C apply Collection only For more info contact our reception 015397834 #giveaway #appointment #routine #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verrucaButton
-
Achilles Tendonitis can be a very painful injury. Plese see our website for more information, www.myfeet.ieButton
-
Christmas gift items available. Treat your lovely one to a special gift. See www.myfeet.ie for more informationButton
-
Christmas gifts availableButton
-
Check out our special offers ✨️ 50% off selected items. WWW.MYFEET.IE #blackFriday #podiatry #clinic #offer #dublinButton
-
Podiatry appointment at one of our south Dublin Podiatry Clinics - Merrion Foot Clinic 🦶 #appointment #routine #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
CPD training day for all our staff 😊 #cpr #cpd #firstresponders #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
We are closed today to facilitate staff training. If you have an emergency please email info@myfeet.ieButton
-
The perfect gift for your loved one 🎁 Gift vouchers are now available on our website myfeet.ie and at our clinics 🦶🏥 6 weeks until Christmas 🎄 #giftcard #present #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
CAOIMHE BYRNES Podiatrist, BSc (Hons) Pod. MChSI. Caoimhe gained her qualification in Podiatric Medicine from the National University of Ireland, Galway with a BSc (Hons) degree and is a member of the Society of Chiropodists and Podiatrists Ireland and CORU. Caoimhe has gained a valuable experience in the care of the diabetic foot, biomechanical assessment and routine podiatry through both placements in Merlin Park Hospital and working in private practice. She has a keen interest in wound care management and the role the podiatrist plays in keeping patients active and pain free. #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
Happy Halloween to all our patients 🎃🧙♀️ #Halloween #spookyfeet #KeepingYouActiveAndPainFree #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
Our treatment room at MerrioFootClinic on Seafield Road 👣 #KeepingYouActiveAndPainFree #clinic #treatmentroom #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
New stock! 👣 Check our online shop - myfeet.ie 😊 #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
Edel Beatty Podiatrist, BSc (Hons) Pod. MChSI. Edel is originally from Galway, qualifying from the National University of Ireland, Galway with a Bachelor of Science (Hons) Podiatry and is a member of the Society of Chiropodists and Podiatrists Ireland. She has gained invaluable experience during both internal and external placements, focusing on routine podiatry care, lower limb biomechanics, wound care, nail surgery and podopaediatrics. She also has a keen interest in diabetes and wound care management. #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
Welcome to our team Triona 😊Button
-
New in stock! DaniPro infused Nail Polish. The only doctor formulated nail polish infused with Undecylenic Acid Safe. Organic. 100% Natural. daniPro is different from other nail polishes. It contains Undecylinic Acid and is completely free of the damaging chemicals found in so many of the popular brands today, including formaldehyde, formaldehyde resin, toluene, or DBP. daniPro has also never been tested on animals. Check our website for more. Myfeet.ie #podiatry #medicalpedicute #pedicure #toxinfree #feet #chiropody #footproblem #pain #podiatrist #fungal #infection #toenails #nails #dublin #stillorgan #clinicButton
-
Swift is the latest and most revolutionary medical microwave technology that is highly effective at resolving verrucas, warts and papillomas 👣 Book your appointment today - online - or call our reception. #KeepingYouActiveAndPainFree #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca #warts info@merrionfootclinic.ieButton
-
Marie O'Connor Podiatrist, BSc (Hons) Pod. MChSI. Marie graduated from the National University of Ireland, Galway with a BSc (Hons) degree in Podiatric Medicine and is a member of the Society of Chiropodists and Podiatrists Ireland. Marie has gained previous experience in all aspects of podiatry including routine podiatric care, diabetic foot care, gait analysis and lower limb biomechanics. Marie has a keen interest in the role a Podiatrist plays in keeping patients active and enjoying life to the best of their ability. #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ieButton
-
WHAT IS SWIFT®? Swift is a new technology, developed in the UK, which has been licensed for the general treatment of skin lesions, warts & Verruca in Podiatry and Dermatology. Swift uses microwave energy which is delivered through a special probe applied to the skin to treat the affected tissue. DOES IT HURT? It is not uncommon for patients to feel a sharp sensation, similar to an injection. Unlike most treatments for verruca, pain felt during the treatment quickly subsides and only lasts a matter of seconds. This is the most up to date technology in the treatment of verrucas. Swift Verruca Microwave Therapy passes cutting edge microwaves safely through the skins layers to ZAP that Verruca, leaving no burns or scarring without using any toxic chemicals allowing immediate return to full activity. There is no need for anaesthetics or pain relief medication. WHAT CAN I DO AFTER TREATMENT? There is no down time after treatment. No plasters. And you can return to activity & sport straight away. In some cases the treated area may feel sore but will not prevent you undertaking normal daily activities. HOW MANY TREATMENTS WILL I NEED? The protocol for Swift treatment is 3 treatments, 4 weeks apart and a follow up appointment 12 weeks after the final treatment. Treatment success was achieved by 83% of patients following these guidelines. As each individual case is different some patients required further treatment after the 12 week period. CAN ANYONE RECEIVE THIS TREATMENT? With a few exceptions, most people with skin lesions would be able to have this treatment. Your Podiatrist will carry out an assessment prior to treatment and be able to advise you on this. #running #backpain #kneepain #Podiatrist #anklepain #southDublin #plantarfasciitis #diabetes #diabetic #podiatrist #podiatryclinic #footcare #prioryfootclinic #southdublin #feetproblems #medical #podiatrylife #heelpainrelief #verruca #verrucas #swifttreatment #plantarfasciitisrelief #Athlone #dublin #footdoc #booterstown #mountmerrion #stillorgan #chiropody #podiatryButton
-
Aishling Forkan Podiatrist, BSc (Hons) Pod. M�ChSI. Aishling graduated from the National University of Ireland, Galway with a BSc (Hons) degree in Podiatric Medicine and is a member of the Society of Chiropodists and Podiatrists Ireland. Aishling has gained previous experience in all aspects of podiatry including routine podiatric care, diabetic foot care, gait analysis and lower limb biomechanics. With her experience in sport, Aishling has a keen interest in the role a Podiatrist plays in sport and the importance of keeping athletes injury free #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ie 01-5397834Button
-
What is Athlete's Foot? Athlete’s foot, also known as tinea pedis, is a fungal infection of the feet, that can affect the skin and nails. Causes? Direct contact with someone with active tinea pedis Thrives in warm, moist, damp conditions increasing the risk of infection in shower rooms, bathroom sand swimming pools Risk Factors: Feet prone to perspiring Sharing socks, shoes or towel with someone with an active infection Keeping feet wet for long periods of time Walking barefoot in public areas - eg. swimming pool, gym changing rooms Symptoms: Fissures or cracks in the skin between the toes Redness and itching between the toes Dry blistering on the feet Discoloured, brittle and thickened toenails Treatment: Over the counter topical antifungal powders and creams - eg. Daktarin In severe cases, a GP may prescribe oral antifungal medication If you feel you have a current fungal infection of the skin or nails, please contact the clinic and make a routine appointment for advice regarding treatment options Aishling Forkan Podiatrist BSc (Hons) Pod. MChSI. #running #anklepain #plantarfasciitis #backpain #bunion #sorefeet #diabeticfootcare #kneepain #KeepingYouActiveAndPainFree #NewPodiatrist #southDublin #healthyfeet #Podiatrist #bunions #heel #Dublin #diabetes #health #foot #diabetic #podiatrist #feet #podiatryclinic #feetcare #shoes #prioryfootclinic #footproblems #feetproblems #southdublin #medicalButton
-
Joe Egan Podiatrist, BSc (Hons) Pod. MChSI. The Priory Foot clinic is owned and run by Mr.Joe Egan. Joe graduated from the National University of Ireland, Galway in 2013 with a BSc (Hons) degree in Podiatry. He is MChSI registered and HSE Approved. He previously worked in musculoskeletal podiatry in clinics based in Ireland. He has clinical experience in podiatry and biomechanics as part of his undergraduate degree. This included placements in several hospitals in Galway, Dublin & Wicklow. Joe see's patients from a wide range of issues, Diabetic Footcare, Podiatry Care, Foot & Ankle Biomechanics and Swift lazer treatment. He has undertaken a dry needling/acupuncture and taping course as part of his continuous development in Podiatry. A keen runner, Joe understands how important it is to be at your very best #KeepingYouActiveAndPainFree #NewPodiatrist #FootCareExpert #sorefeet #Dublin #Podiatric #southDublin #heel #Podiatrist #running #bunions #backpain #bunion #plantarfasciitis #kneepain #anklepain #diabeticfootcare #diabetes #healthyfeet #podiatrist #feet #podiatryclinic #feetcare #footcare #prioryfootclinic #feetproblems #southdublin #plantarfascia #swifttreatment #verruca info@merrionfootclinic.ie 01-5397834Button
-
Our friendly and welcoming staff are always here for you! 😊👣 Happy Tuesday ☺️Button
-
Treat your feet! 👣🌸 book your appointment today ☺️Button
-
*Órla Flood* Podiatrist, BSc (Hons) Pod. MChSI. Órla gained her qualification in Podiatric Medicine from the National University of Ireland, Galway with a BSc (Hons) degree and is a member of the Society of Chiropodists and Podiatrists Ireland and CORU. Órla has clinical experience in many aspects of podiatry including routine podiatry care, diabetic foot care, lower limb biomechanics and a keen interest in wound care management. Órla is committed to providing patient centred care, working with her patients to provide individualised treatment plans to meet their needs As an active person Órla understands the importance of keeping her patients active, pain free and being able to enjoy life to the fullest.Button
-
We are delighted to welcome Caoimhe to our team at Priory Foot Clinic! 🎉 Caoimhe brings a wealth of knowledge and expertise to our practice. She obtained her qualification in Podiatric Medicine from the prestigious National University of Ireland, Galway, with a BSc (Hons) degree. She is also a proud member of the Society of Chiropodists and Podiatrists Ireland and CORU. With her experience in caring for the diabetic foot, conducting biomechanical assessments, and providing routine podiatry services, Caoimhe has honed her skills through placements at Merlin Park Hospital and working in private practice. Her dedication to wound care management and her understanding of the podiatrist's vital role in keeping patients active and pain-free are remarkable. We are confident that Caoimhe's expertise and passion for podiatry will greatly benefit our patients. Join us in extending a warm welcome to Caoimhe as she embarks on this new journey with us! If you would like to book an appointment with Caoimhe or have any inquiries, please feel free to contact our clinic at (01) 539 7834. Let's give a big thumbs up 👍 and welcome Caoimhe to our team! We look forward to the outstanding care she will provide to our valued patients. #WelcomeCaoimhe #NewPodiatrist #FootCareExpert #KeepingYouActiveAndPainFreeButton
-
Interesting facts for our patients who ask about what football boots to purchase #southdublin #podiatry #sorefeet #chiropody #mount merrion #Ireland #podiatricmedicineButton
-
Ccs cream... fantastic product for your dermatology needs of the Feet. Buy online OK our website: www.myfeet.ie #podiatricsportsmedicine #podiatry #podshealheels #chiropody #Dublin #stillorgan #mountmerrion #southdublinButton
-
We are Hiring! Podiatrist Needed for our Athlone Foot Clinic! Please send an email to: joe@merrionfootclinic.ieButton
-
Thank you very much to @orlaflood_ who spent her final year placement from @unigalwaypodmed at our @prioryfootclinic Well done and all the best in your podiatry career. #podiatry #podiatricsportsmedicine #Dublin #sorefeet #insoles #chiropody #stillorgan #mountmerrion #blackrockButton
-
Delighted to have a student from @unigalwaypodmed who will be heading to Tanzania for five weeks to work with The Olive Branch for Childrens “Feet First” Programme. "Hello, our names are Emer, Órla, Eva and Michelle, and we are final year Podiatry students in the University of Galway. This summer, we will be travelling to Mbeya, Tanzania for five weeks to work with The Olive Branch for Childrens “Feet First” Programme. The Olive Branch for Children helps remote communities in Tanzania by assessing their primary needs and establishes programs that target the most vulnerable in those communities. They focus on community health care, HIV/AIDS prevention and care, early childhood education, food security, environmental issues, gender equality, and vulnerable children and women. Their goal is to establish community-led programs that empower remote communities and generate models that can be replicated in communities throughout Tanzania. Health care services are provided by local workers who work with The Olive Branch, to improve the standard of health across the rural Mbeya region. As soon to be qualified podiatrists, we will be volunteering as part of the Feet First Programme, one of many programmes run by the Olive Branch. It not only focuses on the treatment of wounds caused by Diabetes, Leprosy, and other Chronic Illnesses, but also traumatic wounds, caused by minor or major accidents. This programme further provides treatment and management of lower limb problems such as arthritis, neuropathy, plantar fasciitis and fungal infections. There is further provision of at-home services to ensure all patients are able to get the care needed and become healthy and active members of society again. We would appreciate your support through donations and shares and you can follow the link below to learn more about The Olive Branch for Children and their multitude of programs All donations are appreciated and will go directly to The Olive Branch and allow all their local workers to continue their provision of vital health care services, education and community support. Thank you!" https://gofund.me/3bf1227aButton
-
We are Hiring! Podiatrist Needed for our Athlone Foot Clinic! Please send an email to: joe@merrionfootclinic.ieButton
-
Upcoming day with Swift Verruca treatment in our Priory Foot Clinic in South Dublin #verruca #Dublin #podiatry #clinic #mount merrion #stillorgan #podiatricmedicineButton
-
HAPPY VALENTINE'S DAY! Why don't you treat them to something they'll really love? Call the clinic today, on (01) 539 7834, to give your loved one the gift of happy feet.Button
-
Athlete’s foot, also known as tinea pedis, is a fungal infection of the feet, that can affect the skin and nails. Causes? ● Direct contact with someone with active tinea pedis ● Thrives in warm, moist, damp conditions increasing the risk of infection in shower rooms, bathroom sand swimming pools Risk Factors: ● Feet prone to perspiring ● Sharing socks, shoes or towel with someone with an active infection ● Keeping feet wet for long periods of time ● Walking barefoot in public areas - eg. swimming pool, gym changing rooms Symptoms: ● Fissures or cracks in the skin between the toes ● Redness and itching between the toes ● Dry blistering on the feet ● Discoloured, brittle and thickened toenails Treatment: ● Over the counter topical antifungal powders and creams - eg. Daktarin ● In severe cases, a GP may prescribe oral antifungal medication If you feel you have a current fungal infection of the skin or nails, please contact the clinic and make a routine appointment for advice regarding treatment options #merrion #insoles #footclinic #clinic #mountmerrion #stillorgan #chiropody #footdoctor #podiatry #podiatry #podiatrist #podiatrist #podiatryclinicButton
-
HAPPY NEW YEAR! May the coming year be full of opportunities and fruitful encounters. Priory Foot Clinic www.merrionfo#booterstown #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstownButton
-
Diabetes can affect the feet in a number of ways. It is therefore of the utmost importance to have regular appointments and check the feet often. Peripheral Neuropathy: When your blood glucose levels are elevated for an extended period of time it can damage sensation in the peripheries of the body i.e., hands, feet. This damage to nerves can result in a condition called peripheral neuropathy, symptoms of which include numbness, tingling and burning. Patients who develop this are at risk of developing foot ulcers , as they may not feel cuts, blisters and other injuries on the feet. How to Care for Your Feet: -Check them regularly for any abnormalities e.g. Corns, Callus, Cuts, Blisters -Wash feet daily with warm water -Dry between the toes thoroughly as these area can split easily -Do not walk barefoot -Wear well fitting footwear -Speak to your podiatrist about cutting your nails correctly. If you have any impairment to cutting your own nails have a podiatrist to do them for you If you have and questions or concerns regarding your foot health and diabetes, contact your local podiatrist for a consultation. #podiatrist #podiatryclinic #merrion #orthotics #insoles #footclinic #clinic #mountmerrion #stillorgan #chiropody #podiatry #footdoctor #diabetes #diabetic #diabetes #diabeticfootcareButton
-
Sever’s disease, also known as calcaneal apophysis, is one of the most common causes of heel pain in growing children and adolescents. It affects the growth plate, located at the back of the heel where bone growth occurs. It is usually influenced by stress on the body during a growth spurt. Generally affects children between the ages of 8-14 years. Symptoms: Symptoms are often initiated by activities such as running and jumping. Symptoms include pain at the posterior heel, swelling and tenderness. Treatment: Treatment of Sever’s Disease varies depending upon the severity, generally focusing on reducing pain and swelling. It is important to reduce high impact exercise during this time and focus on low impact activity such as swimming. In most cases, symptoms resolve within a few weeks with the correct management. Management: ● Appropriate footwear: Elevation of the heel will reduce pressure exerted on the growth plate ● Gel heel pads: To provide cushioning to the heel and reduce shock absorption ● Anti Inflammatory medication: Ibuprofen, where needed ● Ice: 2 x 10 minutes daily ● Stretching and strengthening exercises: Advised by your Podiatrist with focus on reducing pressure on the growth plates #podiatryclinic #podiatrist #merrion #orthotics #insoles #footclinic #clinic #mountmerrion #stillorgan #chiropody #podiatry #footdoctorButton
-
Merry Christmas! Wishing you a season full of light and laughter for you and your family. Priory Foot Clinic. www.merrionfootclinic.ie #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstownButton
-
Cold weather can be difficult for your body, especially the feet. Low temperatures make it difficult for our body to transport warm blood to the extremities i.e. feet and hands. Therefore it is important to keep them warm in order to prevent injurys due to numb feet and icy paths. It is also important to do this correctly as doing so too quickly may cause burns, blisters or chilblains. Wear warm, breathable socks: Socks which are made of natural fibres ensure the feet do not sweat while in the shoe, encouraging fungal infection. Change the socks throughout the day if they become damp. Boots: Wear a shoe suitable for suitable for the icy conditions outside. A boot will keep your feet dry and protected but will also provide better grip when walking in comparison to a runner. Examples include: Mephisto, Reiker and Dr Marten Slowly Warm the Feet: When coming in from outside it may bne tempting to put your feet in front of the fire/radiator. This rapid heat change can cause our blood vessels to constrict quickly resulting in painful/itchy chilblains. To avoid this make slower transitions from warm to cold i.e. put on a thick pair of socks over placing the feet in front of a direct source of heat. Moisturise: Cold weather can cause our feet to dry and crack. Therefore a urea based moisturiser is an essential during the winter period. Examples include CCS, Eucerin and Silcox Base. #podiatrist #podiatryclinic #orthotics #footclinic #clinic #mountmerrion #chiropody #podiatry #footdoctor #footcare #feetcare #feetButton
-
What is a hammer toe? ●Hammer toe is a foot deformity, caused due to an imbalance in the muscles, ligaments and tendons, that hold the toe in a straight position ● It presents with an abnormal bend in the middle joint of the toe. It most commonly affects the 21nd, 3rd or 4th toe Symptoms: ● Pain: Due to the abnormal bending of the toe ● Corns and callus: due pressure and friction within footwear Causes: ● Footwear: Ill fitting shoes with a narrow toe box eg. high heels ● Trauma: Previous injury or trauma to the toe can leave it more susceptible to developing a hammer toe ● Imbalance between the muscles of the toes, leading to instability and scrunching of the toes Treatment: ● Footwear advice - accommodating footwear with a deep toe box ● Routine care - manage callus and corns forming over the joint ● Padding and strapping - to reduce pressure and friction ● Referral to orthopaedics if neededButton
-
CHRISTMAS IS HERE! ARE YOUR FEET READY? Visit our website for bookings online! LAST APPOINTMENTS AVAILABLE!!! www.merrionfootclinic.ie #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstownButton
-
Shoes play an important factor in our overall foot health throughout all ages, however, as we age, they become more important as the risk of falls increase. Fit: A well-fitting shoe is imperative in the prevention of trips and falls. A shoe that is too big will cause the foot to slip and the heel to lift at the heel counter. A shoe that is too small will cause injury and pain the foot causing the wearer to lose balance during the gait cycle. Grip also plays a role in preventing injury, ensuring a good grip will prevent slipping in the home or outside. Along with this the weight of the shoe should be considered. Heavy shoes will cause a shuffling gait and affect balance during the gait cycle. Checking the Shoe: Check the Heel Counter - is the back of the shoe supportive enough or can I press the heel counter down? Toe Flexibility - is the toe box able to bend? You should have approximately 60° of flexibility at the toe box. Rigidity - can I bend the shoe over on it self? Will the foot be supported in the shoe? The shoe shoe should not bend at the middle. Shoe Examples: · Brooks · Hoka · Asics · Orthofeet · Doctor Comfort · Cozy Feet #footclinic #clinic #stillorgan #chiropody #footdoctor #insoles #podiatry #podiatrist #podiatryclinic #podiatry #shoes #feet #feetcareButton
-
We would like to thank Brian and Seán for the time they spent with us doing the Placement at the Priory Foot Clinic. We enjoyed your presence at the clinic. We wish you all the best in the future.Button
-
What products can you buy in the clinic for Christmas? Christmas is fast approaching! Here are a few simple small gift ideas available in the clinic this Christmas: 1. CCS Cream CCS cream is a Swedish foot care. It is extremely effective in the control of dry and rough skin. It contains 10% urea, needed to soften hard, dry skin to help keep the skin supple. It is recommended by Podiatrists. 2. Tea Tree Oil: Tea tree oil is an essential oil that comes from steaming the leaves of the Australian tea tree. Tea tree oil can be used topically as a naturally antibacterial. It is often used during the treatment of tinea pedis (athlete's foot) and onychomycosis (fungal nails). 3. Mycosan: Topical prevention and treatment for fungal nails. Clinically proven. Comes with a user friendly brush applicator. 4. Mykored: Mykored nail protection oil cares for your nails with specially selected oils and vitamins. It contains clotrimazol, proven to use in the prevention of fungal nails. Suitable for brittle nails. All products are available to purchase at the Priory Foot Clinic.Button
-
Christmas is almost here and if you are still looking for that perfect gift for someone on your list, consider giving the gift of better foot health! Not sure where to begin? We’ve got some great gift ideas that will make your loved ones’ feet feel great. So, check out our top Christmas gift ideas, and feel free to stop in our office for further recommendations or foot care tips! (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Christmas is almost here and if you are still looking for that perfect gift for someone on your list, consider giving the gift of better foot health! Not sure where to begin? We’ve got some great gift ideas that will make your loved ones’ feet feel great. So, check out our top Christmas gift ideas, and feel free to stop in our office for further recommendations or foot care tips! (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Christmas is almost here and if you are still looking for that perfect gift for someone on your list, consider giving the gift of better foot health! Not sure where to begin? We’ve got some great gift ideas that will make your loved ones’ feet feel great. So, check out our top Christmas gift ideas, and feel free to stop in our office for further recommendations or foot care tips! (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Christmas is almost here and if you are still looking for that perfect gift for someone on your list, consider giving the gift of better foot health! Not sure where to begin? We’ve got some great gift ideas that will make your loved ones’ feet feel great. So, check out our top Christmas gift ideas, and feel free to stop in our office for further recommendations or foot care tips! (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
SWIFT TREATMENT Breakthrough treatment is NOW AVAILABLE for stubborn Verruca. Frequently asked questions by patients considering treatment using Swift microwave therapy. WHAT IS SWIFT®? Call the Priory Foot Clinic today to discuss your treatment and to finally say goodbye to your Verruca. (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Successful Swift Verruca Care Results! CASE 2 The patient attended 3 swift appointments over 12 weeks. Call the Priory Foot Clinic today to discuss your treatment and to finally say goodbye to your Verruca. (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
CHRISTMAS IS HERE! Are your feet ready? Whether you're staying in or going out this party season, why not treat your feet with an appointment with our podiatrists? #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Successful Swift Verruca Care Results! CASE 1 The patient attended 3 swift appointments over 12 weeks. Call the Priory Foot Clinic today to discuss your treatment and to finally say goodbye to your Verruca. (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Swift is a new technology which uses microwave therapy in order to treat soft tissue lesions such as verrucas. Through a specialised probe it delivers a precise and highly controlled dose of microwave energy. This allows the treatment to travel and treat infected tissue which can exist several millimetres below the skin surface (making it difficult to treat through traditional methods i.e. salicylic acid). Swift stimulates an immune response, therefore treating the root cause of the verruca (HPV). The efficacy of Swift is significantly higher compared to other treatments available. Who can receive Swift treatment? Most people are eligible to receive Swift treatment, however, there are a few exceptions. Your podiatrist will carry out an assessment of this on your consultation. What to Expect: Our protocol for this treatment is 3 treatments spaced 4 weeks apart with a follow up appointment 12 weeks following the final treatment. This number can vary depending on the lesions' response to treatment. Factors such as length of time the verruca has been in place or its size can affect this - each individual case is different and your clinician will be able to guide you on this. The treatment takes just minutes and requires no dressings / anaesthesia / at home treatments between appointments. Pain is variable and patient specific, minor discomfort is to be expected with most describing it like an injection or burning feeling. This pain lasts a short while and immediately subsides upon cessation of the treatment and there is no prevention to return to daily activity. If you suspect you have a verruca contact a podiatrist as soon as possible. Symptoms include: www.merrionfootclinic.ie 01-5397834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown Localised pain Tenderness on compression of the sides of the lesion Rough skin with small black dots within it / this may appear alone or in a clusterButton
-
SWIFT TREATMENT Breakthrough treatment is NOW AVAILABLE for stubborn Verruca. Frequently asked questions by patients considering treatment using Swift microwave therapy. WHAT IS SWIFT®? DOES IT HURT? WHAT CAN I DO AFTER TREATMENT? CAN ANYONE RECEIVE THIS TREATMENT? Call the Priory Foot Clinic today to discuss your treatment and to finally say goodbye to your Verruca.. (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
SWIFT TREATMENT Breakthrough treatment is NOW AVAILABLE for stubborn Verruca. Call the Priory Foot Clinic today to discuss your treatment and to finally say goodbye to your Verruca.. (01) 539 7834 #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstown #verruca #swift #swifttreatmentButton
-
Visit our website for bookings online! www.merrionfootclinic.ie #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstownButton
-
https://www.justgiving.com/fundraising/michael-o-shea3 Best of luck Michael and Jarlath from all at the @Merrion foot clinic in todays Dublin City Marathon 2022 All in aid of a great cause MND. Please give as generously as you can #merrion #orthotics #insoles #footdoc #footclinic #clinic #mountmerrion #booterstown #stillorgan #chiropody #footdoctor #mnd #motorneuronedisease #motorneurondiseaseButton
-
All ready, just waiting for our patients now ☺☺Button
-
What is it? Metatarsalgia is a condition in which the ball of the foot becomes inflamed and painful. What causes it? ● High impact activity or training load - eg. running, as the ball of the foot absorbs significant force when making contact with the ground ● Foot type - Pes Cavus foot type (high arch) or a 2nd toe that is longer than the big toe (hammer toe) ● Ill- Fitting Footwear - Shoes with a narrow toe box can add excessive pressure to the ball of the foot ● Excess weight - can add excessive pressure to the forefoot Signs & Symptoms ● Sharp, aching, shooting pain in the ball of the foot ● Numbness/tingling in the toes ● Pain that worsens upon weight-bearing and improves with rest ● The sensation of having a pebble in your shoe What can we do? Conservative management of the presenting symptoms. ● Rest/reduction in activity - for the recommended period of time ● Advice regarding suitable footwear - that offer adequate cushioning to the forefoot and have a wide toe-box ● Custom orthotics - to relieve the symptoms and deflect stress from the area ● Ice - 10 minutes twice dailyButton
-
What is it? Sesamoiditis is inflammation of the tendons attached to the sesamoid bones, located at the base of the big toe (as shown in the image attached). Sesamoid bones act like a pulley, allowing the tendons to run smoothly over the joint. What causes it? ● Sesamoiditis is caused due to overuse of tendons associated with the sesamoid bones ● Ill fitting footwear can result in repetitive trauma to the tendons eg. High heels ● High impact activities eg. Running, basketball Signs & Symptoms ● Inflammation and swelling ● Bruising ● Pain at the big toe joint ● Difficulty bending or straightening the big toe What can we do? ● Reduce activity for the recommended time ● Ice the area twice daily for 10 minutes to reduce inflammation ● Advice regarding the necessary footwear to offer cushioning and support ● In some cases, taping may be necessary to relieve pressure on the toe #merrion #footclinic #clinic #mountmerrion #stillorgan #chiropody #footdoctor #feet #prioryfootclinic #footproblemsButton
-
What is it? In simple terms, turf toe is a sprain of the main joint of the big toe. Ligaments, soft tissues and tendons can stretch or tear. It commonly occurs among footballers and athletes who sprint or jump. What causes it? This can happen when you bend your big toe too far or too forcefully (hyperextension). The big toe is usually bent at a 90 degree angle and pressed flat against the ground. When pushed too far, this motion causes soft tissues and ligaments (connect bone to bone) to be stretched or torn (sprain). This injury can result from a sudden trauma such as athletes who make sudden foot movements and changes in direction eg. Sprinters. In this case you may have heard or felt a sudden “pop” when the injury happened and pain will come on immediately. Turf toe can also result from many repetitive movements over time eg. Ballet dancers. These symptoms will usually develop gradually and get worse over time. What can we do? We will take a thorough history of your symptoms, ask how it happened, how long the symptoms have been present, where you feel pain etc. This guides us in how we will proceed and diagnose the injury. we will examine your toe and check the area for tenderness and also assess the ROM. Based on our findings we may order an X-ray or MRI scan to check for damage in the bones, ligaments and tendons. Signs & Symptoms ? Turf toe symptoms can range from mild to severe. -Pain and tenderness: this may be constant or only when you put pressure on the affected area. -Swelling and bruising: swelling may occur around the base of the big toe and sometimes extend to the top of the foot -Limited Range of Motion (ROM): you may notice weakness in the big toe joint when pushing off the ground. You may not be able to bend your toe up or down like before. -Joint that feels loose: the MTP joint may pop out of place or feel like it’s unstable. It also may feel stiff #footdoctor #chiropody #stillorgan #mountmerrion #clinic #footclinic #podiatry #podiatrist #podiatryclinic #feet #feetcareButton
-
What is it ? Trench foot, aka immersion foot syndrome, is a type of tissue damage caused by prolonged exposure to cold, damp and wet conditions. If left untreated it can lead to damage of the nerves, blood vessels, skin and muscle. It is different to frostbite in that it is a non-freezing cold injury. What Causes it? Changes in circulation (blood flow) to the feet- usually due to cold temperatures which leads to constriction of the blood vessels in the feet Pressure - standing still in one position for long periods of time can contribute to trench foot as it impedes blood flow through the feet Excessive sweating/wearing damp socks - trench foot can occur in any damp environment where the feet are constantly wet for a prolonged period. Unlike frostbite it can develop in temperatures up to 16 degrees. Common in builders, hikers, security guards, campers, festival goers What can we do? Thorough medical history take Assess for signs and symptoms of trench foot Advise on treatment methods Advise on prevention methods to avoid reoccurrence Refer on to other professionals if needed- such as GP, dermatology Signs & Symptoms? - Tingling and itching - Pain - Swelling - Cold blotchy skin - Numbness - Prickly or heavy feeling in the feet - Soles of feet can be wrinkled, skin can appear damaged #footclinic #clinic #chiropody #footdoctor #feet #feetcare #feetproblems #podiatry #podiatristButton
-
What is it? Foot drop is described as a difficulty to lift or move the foot and toes. It is more often a unilateral issue meaning it only affects one foot. It can cause the person to drag their foot when walking. Causes: Foot drop is commonly caused by an injury to a nerve that controls the muscles which lift the foot (peroneal nerve injury). These can include Damage During hip/knee replacement surgery Nerve damage related to diabetic neuropathy Sports injury Compression of nerve Brain / Spinal cord disorders i.e. stroke, cerebral palsy, multiple sclerosis Signs and Symptoms: High instance of tripping/falls Steppage gait - raising the thigh as you are walking (like climbing stairs) to aid in ground clearance Numbness or tingling in the leg or foot Decrease in muscle mass due to weakening of muscles Circumductive gait - leg remains straight while swinging outward to move forward Treatment: Physical Therapy Nerve Stimulation Surgery Podiatric Intervention: Bracing or splint A brace or splint which has been fitted to the ankle and foot and fits into the shoe can help to hold the foot in a corrected position. It is indicated for use in patients unsuitable for surgical intervention or looking for a non-invasive treatment for foot drop.Button
-
What is it? This type of injury results if bones in the midfoot are broken or ligaments that support the midfoot are torn. The midfoot is the middle region of the foot where a cluster of small bones form the top of the arch. These bones are then held in place by a number of strong ligaments known as the Lisfranc joint complex. The severity of this injury can vary widely depending on whether just one or multiple joints are affected. What Causes it? A mild Lisfranc injury can occur as a result of a simple twist or fall, often seen in football or soccer players where the is force applied to the back of the foot while in a downward flexed position. Known as a low-energy injury. More severe Lisfranc injuries tend to occur as a result of direct trauma such as a fall from a height or collision. Multiple joint fractures and dislocations can occur in these instances. Known as high-energy injuries. What can we do? Take a medical history: talking about the symptoms you're experiencing and discussing your concerns Physical examination of the foot and ankle: a number of physical tests may be carried out to assess whether or not there may be a fracture or ligament damage Referral for necessary tests: such as an X-ray to diagnose broken bones or an MRI to diagnose soft tissue injuries such as torn ligaments. Signs & Symptoms? - The dorsal aspect (top) of the foot may be tender to touch and swollen - There may be bruising on the top and/or bottom of the foot. Bruising on the sole of the foot is particularly indicative of a Lisfranc injury - Pain in the midfoot region that worsens with standing, walking or performing the toe-off motion - Pain may be so bad than weight-bearing is not possibleButton
-
For many parents it is coming up to that time of year where it is time to buy your children’s back to school shoes. It is important to consider a few things when doing this: Tips When Buying A New Shoe: * It may be tempting to buy a shoe that is larger then what your child needs for “growing room”, however these can be a tripping hazard / cause rubbing or blistering - There should be a thumbs width room at the top of the shoe to account for growth and allow space for the foot to move * Measure both feet - it is common for one foot to be larger/smaller then the other Checking the Shoe: 1. Check the Heel Counter - is the back of the shoe supportive enough or can I press the heel counter down? 2. Toe Flexibility - is the toe box able to bend? You should have approximately 60° of flexibility at the toe box. 3. Rigidity - can I bend the shoe over on it self? Will the foot be supported in the shoe? The shoe should not bend at the middle. Regularly check your children’s shoes during the year to ensure the fit is correct. If your child has any unexplained foot pain or irritation a visit to your local podiatrist may be advised to rule out any footwear related issues.Button
-
Custom insoles. A busy day here in the Priory Foot Clinic with our custom insoles. If you are interested or in need of custom orthotics please contact us today for book a full biomechanical appointment with one of our SCPI registered Podiatrist. 🖥 Www.merrionfootclinic.ie 📲 01-5397834 #podiatryonline #podiatrist #podiatry #southdublin #blackrock #footdoctor #stillorgan #mountmerrion #feet #footpain #planterfasciitis #footdoctor #heelpain #insoles #orthotics #footwear #runners #sorefeetButton
-
We would like to celebrate with you that our Mount Merrion Clinic has moved across the N11 to our new state-of-the-art Foot & Ankle Podiatry Clinic. The Priory Foot Clinic opened its doors this week. We are in the Priory Office Park, just next to the Talbot Hotel on the N11. New Address: 14 Priory Office Park, Stillorgan Road, Blackrock, Co. Dublin A94 T671 We want to celebrate this news with you with this competition WIN a voucher for €150, for AMPHIBIAN KING To take part in the competition: 1.- Follow our Instagram page @merrionfootclinic 2.- Share this post on your Instagram Story 3.- Tag three friends in the comment below The competition closes on Friday 15th of July at @5pm One winner will be chosen randomly. #podiatry #podiatrist #feet #footcare #footpain #leg #leglengthdiscrepancy #foot #heelpain #diabetes #orthotics #plantarfasciitis #health #podiatrylife #footdoctor #running #medical #ireland #healthyfeet #nails #podsfixfeet #podologo #chiropody #toenails #diabeticfootcare #footandankle #medicine #insoles #plantarfasciitis #heelboneButton
-
New location Our Mount Merrion Clinic has moved across the N11 to our new state of the art Foot & Ankle Podiatry clinic. The Priory Foot Clinic opened its doors this morning for its first patients. We are delighted to share this news with you today and we will keep you posted as the days pass. We are located in the Priory Office Park- just next to the Talbot Hotel on the N11. 01-5397834 www.merrionfootclinic.ie #Podiatry #stillorgan #footclinic #mountmerrion #footdoctorButton
-
What are the Consequences of Untreated Plantar Fasciitis Plantar Fasciitis (PF) is an inflammation of the fibrous band of tissue - the plantar fascia - which runs along the plantar aspect of the foot, inserting at the heel bone. This is caused by repetitive overstretching of the fascia causing micro tears to the area. This can be diagnosed and treated by a podiatrist. However if PF is left untreated it can lead to a number of issues which can cause chronic heel pain. • Heel Spurs - This is the most common consequence of untreated PF. This is a bony-like growth which occurs as the body responds in order to protect the foot and lessen damage. Calcium is deposited in the area which gradually accumulates into sharp growths at the heel. • Plantar Fibromatosis - Benign nodules which grow slowly along the fascia, possibly caused by tears in the fascia which have been left untreated. These can initially be asymptomatic but as they grow may become painful to walk on. • Plantar Ruptures - Plantar ruptures can be caused by acute injuries such as a sharp blow to the foot however untreated PF combined with continuing high impact activities is a common cause. You may hear a loud pop followed by intense, swelling and bruising if a rupture occurs. You should seek immediate medical attention if you believe you have ruptured your PF. If you have any concerns regarding plantar fasciitis or any of the secondary issues which can occur as a result you should make an appointment with a podiatrist for assessment. By: Marie O’Connor Podiatrist, BSc (Hons) Pod. MChSI. #plantarfasciitis #footpain #heelpain #footcare #kneepain #flatfeet #orthotics #podiatry #running #podiatrist #bunions #foothealth #feet #backpain #bunion #foot #anklepain #insoles #health #healthyfeet #footcareforeverybody #sendalkesehatan #healthyshoes #drkongid #dublin #merrion #booterstownButton
-
WIN a double ticket for Board Bia BLOOM, Ireland's largest and most spectacular gardening event. To take part in the competition: 1.- Follow our Instagram page @merrionfootclinic 2.- Share this post on your Instagram Story 3.- Tag a friend you would like to visit the festival with. The competition closes on Thursday 2nd of June at @5pm One winner will be chosen randomly. #podiatry #podiatrist #feet #footcare #footpain #leg #leglengthdiscrepancy #foot #heelpain #diabetes #orthotics #plantarfasciitis #health #podiatrylife #footdoctor #running #medical #ireland #healthyfeet #nails #podsfixfeet #podologo #chiropody #toenails #diabeticfootcare #footandankle #medicine #insoles #plantarfasciitis #heelboneButton
-
Amy graduated from the National University of Ireland, Galway with a BSc (Hons) degree in Podiatric Medicine and is a member of the Society of Chiropodists and Podiatrists Ireland. Since graduating Amy recognises the importance of keeping up to date with the latest Podiatric developments and so regularly attends course days. Most recently Amy has attended a Biomechanics Masterclass and the Transatlantic Wound Science / All Ireland Podiatry Conference. Amy has gained experience in both private practice and hospital settings across Ireland and enjoys volunteering with the Special Olympics Fit Feet campaign. This experience has given her the knowledge and skills to treat and manage a wide range of podiatric conditions including routine care, diabetic foot care, gait analysis and biomechanics.Button
-
The Most modern treatment available for Verruca Warts in Ireland Swift Laser Treatment WHAT IS SWIFT? Swift is a new technology, developed in the UK, which has been licensed for the general treatment of skin lesions, warts & Verruca in Podiatry and Dermatology. Swift uses microwave energy which is delivered through a special probe applied to the skin to treat the affected tissue. Location Dublin Contact 01-5397834 #merrion #orthotics #insoles #footdoc #footclinic #clinic #mountmerrion #booterstown #stillorgan #chiropody #heelpain #heelpain #heelpainsucks #heelpainrelief #plantarfascia #plantarfasciitis #plantarfasciitisrelief #verruca #verrucas #swifttreatmentButton
-
Delighted to have Student Amy Ronan from NUI Galway today with our in Clinic Podiatrist Amy Todd. Some MSK peer reviews made for some interesting discussions on Plantar Fasciitis #merrion #orthotics #insoles #footdoc #footclinic #clinic #mountmerrion #booterstown #stillorgan #chiropody #footdoctor #heelpainrelief #plantarfasciitis #heelspurs Info@merrionfootclinic.ie 01-5397834Button
-
CASE STUDY Gender: Female Age: 50 Presenting complaint: HAV bilaterally and pes planus foot type Treatment: Orthotic Therapy This patient presented with a painful bunion (HAV) and a pes planus foot type (flat foot type). A full biomechanical assessment was carried out and orthotic therapy was the best treatment option for this particular patient. A cast of the feet were taken in order to create a pair of custom made orthotics to treat this patients pain and discomfort. Also footwear advice was given to the patient, to look for shoes with a wide toe box and good shock absorption; such as Brooks, Hokas or ASICS. By: Amy Ronan Podiatrist StudentButton
-
Plantar fasciitis What is plantar fasciitis? Plantar fasciitis is a disorder of the plantar fascia, which is the connective tissue that supports the arch of the foot. It results in pain in the heel and bottom of the foot that is usually most severe with the first steps of the day or following a period of rest. What causes plantar fasciitis? Plantar fasciitis is caused by increased pressure such as from long periods of standing, an increase in exercise, and obesity. Plantar fasciitis can also be caused by overuse of the ligament from wearing old and unsupportive footwear. What are the treatment options available for plantar fasciitis? Anti-inflammatory medication such as ibuprofen and naproxen can ease pain and inflammation caused by plantar fasciitis. Orthotics custom-fitted or off-the-shelf arch supports can be used to distribute the pressure on your feet more evenly. Physical therapy exercises to stretch the plantar fascia can be used to strengthen muscles in the lower leg which can help with stretching your calves and the plantar fascia itself helps loosen the muscles and reduce heel pain. Taping can also be used to support the bottom of the foot.Button
-
We would like to welcome Geraldine Hackett to the Foot Clinic team. She will be assisting you Mondays and Tuesdays from 8:00 to 15:00Button
-
First session about to start Chaired brilliantly by Emily Haworth International Speakers and Our Chairs, Roisin Connell, Joe Egan and Paddy Kenny Superb SessionButton
-
Achilles Tendinitis Part 1 #podiatry #podiatrist #feet #footcare #footpain #Achillestendinitis #Achilles #Tendinitis #foot #heelpain #diabetes #orthotics #golf #health #podiatrylife #footdoctor #running #medical #ireland #healthyfeet #nails #podsfixfeet #podologo #chiropody #toenails #diabeticfootcare #footandankle #medicine #insolesButton
-
The 5th transatlantic wound science & Podiatric Medicine Conference and The All Ireland Podiatric conference Joe is in attendance the 3 day conference in Co. Galway #podiatry #merrionfootclinic #nuig #galway #footclinic #DublinButton
-
Apical Hard Corn Follow us on TikTok @podiatryclinic for more videos #podiatry #podiatrist #feet #footcare #footpain #apicalhardcorn #hardcorn #corn #foot #heelpain #diabetes #orthotics #plantarfasciitis #health #podiatrylife #footdoctor #running #medical #ireland #healthyfeet #nails #podsfixfeet #podologo #chiropody #toenails #diabeticfootcare #footandankle #medicine #insolesButton
-
Leg Length Discrepancy Part 1 Follow us on TikTok #podiatry #podiatrist #feet #footcare #footpain #leg #leglengthdiscrepancy #foot #heelpain #diabetes #orthotics #plantarfasciitis #health #podiatrylife #footdoctor #running #medical #ireland #healthyfeet #nails #podsfixfeet #podologo #chiropody #toenails #diabeticfootcare #footandankle #medicine #insolesButton
-
What a fantastic evening we had out @mulberrygarden in Donnybrook. #podiatry #podiatrist #merrion #merrionfootclinic #footclinic #dublin #donnybrook #mulberrygardenButton
-
Sever's Disease is a very common cause of heel pain in children and teenagers during growth spurts especially if they are involved in a sport that involves running and jumping. It is also known as calcaneal apophysitis and occurs due to inflammation of the growth plate where the calf and Achilles tendon attach to the calcaneus or otherwise known as the heel bone. Symptoms of Sever's Disease include; • Pain around the heel which may be tender to touch with some swelling • If very painful it can lead to 'toe walking' or a limp due to compensation • Increased pressure from very flat shoes or with a rigid back may increase symptoms • Activities involving repetitive stress such as running and jumping often provoke the pain further. A biomechanical examination is normally required to diagnose Sever's Disease. This involves the Podiatrist discussing the patient's symptoms, and relevant medical history and carrying out assessments to see how the foot and lower limb are functioning. The Podiatrist will often apply pressure to the calcaneal bone and it often feels tender to touch. Treatment of Sever's Disease varies depending on the severity, in most cases symptoms resolve within a few weeks with the correct management. Supportive footwear, a temporary reduction in intense activity, icing the area, anti-inflammatory's and calf muscle strengthening exercises are often used as part of the treatment of this condition. In more severe cases an orthotic may be required to resolve the symptoms. By: Siobhan Ryan Podiatrist, BSc (Hons) #podiatry #clinic #dublin #chiropody #stillorgan #mountmerrion #booterstown #footpain #flatfeet #ireland #heelpain #foothealth #footfixer #footdoctor #blackrock #merrionfootclinic #Athlone www.merrionfootclinic.ie Email info@merrionfootclinic.ie 📧 Call 01 539 7834 ☎️Button
-
Biomechanical Foot & Ankle Assessment this morning at the Merrion Foot Clinic Case Study sex: M Age:61 Presented with unilateral heel pain to the Right heel. Approx. 6 weeks in Duration. Previous treatment- Ball- Ice - Rest. Pain on Palpation of the Pantar Fascial Band to the medial aspect of the heel. Treatment Footwear with @Brooks runners, Insoles @Firefly orthotic Sligo, and exercises for 6 weeks. #merrion #orthotics #insoles #footdoc #footclinic #clinic #booterstown #mountmerrion #stillorgan #chiropody #footdoctor Www.merrionfootclinic.ie Info@merrionfootclinic.ie 01-5397834Button
-
Worried about Osteoporosis in your feet? Here are a few tips to keep your feet and bones healthy! Osteoporosis is a disease of gradual loss of bone density and can progress slowly over years. Ensuring you consume enough calcium and vitamin D on a daily basis is crucial to prevent osteoporosis from developing over time. Book your first podiatry appointment now! #podiatry #clinic #dublin #chiropody #stillorgan #mountmerrion #booterstown #footpain #flatfeet #ireland #heelpain #foothealth #footfixer #footdoctor #blackrock #merrionfootclinic #Athlone www.merrionfootclinic.ie Email info@merrionfootclinic.ie 📧 Call 01 539 7834 ☎️Button
Our Priory Foot Clinic, Stillorgan, Dublin
Quick Links
Get Social
CLINIC Locations
Merrion Foot Clinic,
23 Seafield Rd,
Trimblestown, Blackrock,
Co. Dublin, A94 DX27
Athlone Foot Clinic
Unit 2, 95 Sean Costello St, Athlone, Co.Westmeath, N37 XE08